NCTracks Common Questions: Management Fees: What are they and why are they on my RA?
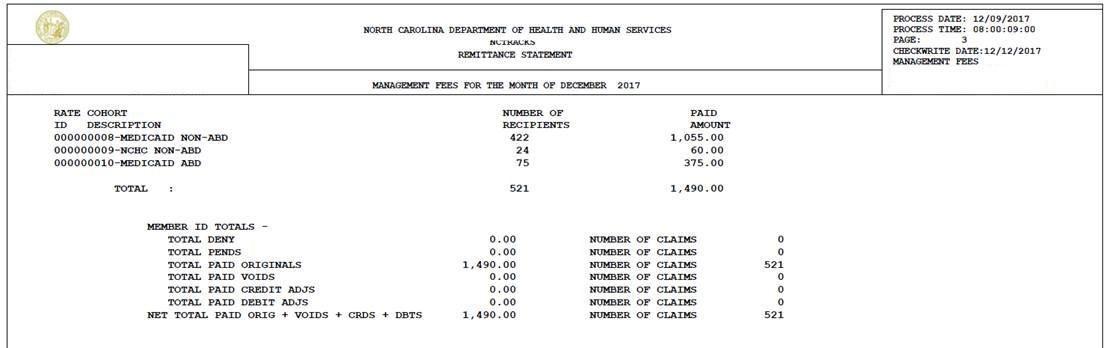
Some primary care providers (PCPs) may have seen an additional payment titled “Management Fees” on their Remittance Advice (RA).
This fee is an additional compensation per Medicaid beneficiary. PCPs participating in the Community Care of North Carolina (CCNC) network are paid an enhanced per member per month (pmpm) care management fee for each assigned beneficiary.
There is a separate section on the RA for Carolina ACCESS (CA) management fees that includes:
• Dates of service
• Rate cohort code and description
• Paid amount
• Number of claims
Please see the RA screenshot attached for reference.
The enhanced fees are noted as follows:
|
ABD Medicaid Beneficiaries (Aged, Blind, Disabled) not eligible for Tailored Care Management |
$5.00 |
|
Non ABD Medicaid Beneficiaries not eligible for Tailored Care Management |
$2.50 |
|
NC Health Choice Beneficiaries not eligible for Tailored Care Management |
$2.50 |
|
Medicaid and NC Health Choice Beneficiaries eligible for Tailored Care Management |
$20.00 |
Providers currently enrolled in NCTracks as a NC Medicaid Primary Care Provider who wish to join the CA program may submit a Managed Change Request (MCR) accessing NCTracks. The submission will be reviewed to ensure all qualifications are met.
For more information on CCNC/CA, please see Medicaid’s webpage and article.
 NCTracks
NCTracks